Currently there are two large over arching philosophies on how to treat women during birth. Do you know which one best matches you? Do you know which one best matches your doctor or midwife?

Knowing the answer to those questions can go a long way in creating a positive and satisfying experience when you are in labour. So while you are pregnancy, make sure that you are having those conversations with your care provider and make sure to choose someone who is on the same wavelength as you are.
Active Management of Labor—AML
Active Management of Labor was developed in the 1960s and 70s in Ireland in an attempt to reduce the number of cesarean sections. It was assumed that mothers who had long labours were traumatized. Initially, a normal birth, according to AML standards, was about 24 hours. Over the years that timeline has been considerably shortened to 12 hours. AML has not decreased the cesarean rate; but, instead, has had the opposite effect, with early and routine intervention and drastic steps to bring about a timed and managed labor.
Not all hospitals, doctors, or midwives engage in the Active Management of Labor procedures or protocols. As recommended by the World Health Organization, some providers refrain from this approach unless the birthing circumstances deem it necessary. However, a very large percentage of hospital facilities and care providers today are using some or all features of AML rather than exercising patience and allowing labor to play out naturally.
It also should be noted that, in a normal birth, not all mothers will experience all of the interruptions or interventions that are discussed here.
This is a fictional scenario; but like the television show “ER,” this scenario will acquaint the reader with the many different kinds of procedures that are needlessly imposed and that can turn birth into a most unnatural experience. Birth Preferences are nonexistent.
What might be expected in typical Active Management of Labor (AML) in a hospital setting.
- Induced initiation of labor. If a woman has hired a provider who is impatient, or who subscribes to AML, she may find herself talked into an induction for any number of reasons and at any point during the last three weeks of pregnancy.
- She is “over-due”– her pregnancy has gone beyond the EDD.
- She’s “cooked” and doesn’t need to go through the burden of being pregnant any more.
- She is suspected of carrying a baby who is too big for the size of her pelvis. Baby will continue to get bigger if induction is not initiated she is told. It is very rare for a mother to ‘grow’ a baby that is too big for her to birth.
- She has too little—too much–amniotic fluid
- Her doctor is going out of town and can induce ahead of time if the birthing mother wants to be sure that this doctor “delivers” her baby.
- Methods of induction:
- Rupture of membranes
- Insertion of prostaglandin Gels, Cytotec/ Misoprostil, Cervadil
- Sweeping or stripping of membranes
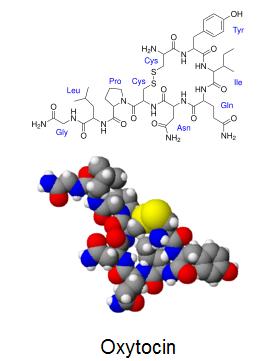
- Infusion of synthetic oxytocin (Pitocin/Syntocinin)
- C. Entry to the hospital:
If a woman is not induced and experiences release of the amniotic membranes as the first sign of labor, often she will be advised to come into the hospital to be checked to determine if there is meconium in the fluid. This often is a lead in for an induction, since she is “there.”
Meconium or not, she will be prompted to accept admission, so that she can be “holding her baby in a matter of hours.” To go to the hospital to be checked often means “checked in.”
Regardless of when she enters the hospital, she will be provided a faded, gray-green, hospital gown to wear–the first step on the way to losing one’s identity. She now “looks and feels like a patient”, and her ego is diminished.
She, like all birthing mothers, will be belted for the mandatory 20-minute strip on the external fetal monitor to determine the base for the baby’s heart rate. She will have an IV, or a heparin lock (IV catheter not hooked up to IV fluids) is inserted, and she will be told that it is to assure that she remains hydrated and so that she can receive other drugs later, should the situation call for them.
She will be tethered by belts to an “external fetal monitor” (EFM) so that baby’s heart rate can be monitored to assess how well he or she is tolerating labor. This keeps her in bed with limited mobility unless the belts are removed.
In spite of her early release of membrane, she will be given several vaginal exams to determine if thinning and opening are taking place.
She will be advised that because her membranes have released, she is in danger of developing an infection that could be harmful to the baby, and she is now on the clock. If her surges don’t start and form a pattern within a “reasonable amount of time,” she is told that she will have to have her labor induced. The amount of time the caregiver will wait can vary from 3 hours to 8 hours. Some care providers will allow a longer time, but will insist on administering antibiotics. She continues to have vaginal exams so that staff can “know” where she is in her labor.
If she arrives at the hospital in labor and her membranes are still intact, they may be ruptured by the caregiver in an effort to speed up her labor.
If labor does not start, a synthetic oxytocin (Pitocin/Syntocinin) is usually the drug of choice to “jumpstart labor.” If she arrives late in the afternoon or in the evening, she may be given a prostaglandin gel medication that will “ripen” the cervix so that she can be induced the following morning.
In some cases, if she is uninformed about drugs, she will accept an agent inserted into her vagina—Misoprostil/Cytotec–a medication that if not carefully monitored, can bring the force of her surges to a tetanic state (continuous spasm brought on by over stimulation from the drug), where surges are fast, hard, difficult to tolerate for both mother and baby, and, if not kept in check, can result in fetal distress and even uterine rupture. While Pitocin, if it is “cranked up too much, can give the same effect, it can be turned off because it is given intravenously. Cytotec cannot be removed or turned off. In spite of the fact that Cytotec is not approved by the FDA for use in pregnancy, it is commonly used to induce labor.
By this time, she will have been offered drugs, such as Nubain, Stadol, or Fentanyl so that she can be relieved of the increased pain caused by the drug that was brought on by the induction. If her baby is born before these drugs metabolize, the baby could have difficulty in breathing.
She will most likely be given an epidural, (anesthesia inserted into the epi space over and around the dura of the spine), which will require that she remain in bed and limit her activity, as well as her ability to breathe through the surges. Often she will have a blood pressure cuff on throughout labor only because it has not been removed.
She will be expected to continue to thin and open—often following the obsolete Friedman’s Curve of one cm. an hour. The dosage of synthetic oxytocin will be increased, especially now that she has the epidural.
The epidural can cause her labor to slow; and in spite of all efforts, she may hear that she needs to have the baby “taken” because of failure to progress. She will have her baby surgically removed. –Or—
She may even develop a fever from the epidural; in which case, she will immediately be taken for a surgical birth. Her baby may become distressed, with a decline in heart rate, and there will be the same result—surgical birth.
If she has no adverse effects from the drugs, but it is determined that the baby is in occiput posterior (OP), facing front, position or in another position that could delay birthing, she will be rushed to the operating room to experience a surgical birth.
If she escapes all of the things that could interfere with her having a vaginal birth, she will eventually reach completion, and will be informed that she can now help herself by “pushing her baby out.” She has reached the second stage of labor.
At this point, the birthing couple will become aware that the attending staff takes over the birthing in every sense, from dictating how the woman will position herself, to how she will breathe, and how she will move her baby down to crowning.
In spite of studies that indicate that pushing is contraindicated for bringing the baby down the birth path, she will be directed, in cheerleader style, to take in a deep breath and hold it for ten seconds while pushing down with all her might. Those around her call out numbers and instruct her to take a second breath when the ten-second count is over.
She is now engaged in forced pushing or valsalva pushing (also called purple pushing) as she pushes down into the birth path to move the baby along.
All the time she is doing this, she is told to push with all of her might “down to where the pain is” and to expect that she will push through a “ring of fire,” as the tissues and rim of the perineum stretch open. This part of birthing can last anywhere from minutes to several hours, mostly because when using forced pushing, she is closing the sphincters of the vaginal outlet ahead of the baby. This kind of pushing reduces the flow of oxygen to the baby, and his heart rate may decline—deceleration. If this happens, there will be talk of the need to get “that” baby out.
If her baby doesn’t descend as quickly as attendants would like to see it descend, several different scenarios could occur.
- It could be determined that the baby is in occiput posterior position, and she will be prepared for a surgical birth, known as Cesarean Section.
- If the baby has descended only somewhat into the birth path, or if the cervix becomes swollen from the forced pushing, the birth may need to be assisted by vacuum extraction or ventouse. This most often requires that the attendant cut an episiotomy, cutting into the muscle tissue of the perineum, to insert the vacuum and extract the baby, or—
- It will be decided that the baby is “stuck” and must be removed by surgical birth, or—
- Exhausted from all the forced pushing and tugging, the baby may experience a decrease in oxygen, along with deceleration of the fetal heart rate. (FHR), and both mother and baby will be whisked away to the operating room for a surgical birth.
Once the baby is born, the umbilical cord will be clamped almost immediately, and the father will be invited to cut the cord. Mother will receive a shot of synthetic oxytocin to cause the placenta to disengage from the wall of the uterus, and to avoid hemorrhage. The attendant will “repair” the episiotomy.
Mom may or may not be able to enjoy that first gaze and bonding with her baby. Baby will have all that wonderful vernix scrubbed from his body and may be taken away while staff performs administrative tasks like weighing, cleaning, banding, and completing APGAR testing while mom and dad look on from a distance across the room.
A neat, clean, swaddled baby will be returned, fully dressed, which precludes skin-to-skin bonding, and the couple is left to become acquainted with this little bundled joy.
The outcome is considered a success because the only real thing that matters is that we have “a healthy mother and a healthy baby.” The birthing may even be considered “natural” if mom is able to birth vaginally, in spite of all of the interventions.
Exhausted from all of the turmoil, the baby may or may not be interested in taking to the breast for his first feeding.
What might be expected in typical Normal, Gentle, Physiologic Birth – HypnoBirthing®
HypnoBirthing has two phases
A. Thinning and Opening
B. Birthing
Moving through a HypnoBirthing
Mother may have one, two, all, or none, of the traditional starts to birthing. For most, the goal is that the start of labor will be spontaneous, rather than induced. She will want to know the medical reason and the alternatives before accepting an induction proposal.
Frequently the only sign of labor for a HypnoBirthing mom is a strange tightening feeling across her abdomen; or she may feel the pressure that is similar to that of constipation; or she may have a low pelvic discomfort similar to light menstrual cramps. For many women, these first signs of labor start at approximately 5 to 7 minutes apart.
The couple will usually stay at home and practice their relaxation material. Some may go about their regular routine, particularly if they have other children. They do not rush to the hospital.
Very often the mother will relax in a tub. She will use these early surges to get into the pattern of relaxation that will carry her through labor. She will eat and move around. She will relax to the Rainbow Relaxation CD and the Birthing Affirmations.
If she experiences SROM, (spontaneous release of membranes) she will check to be sure that the fluid is clear, with no odor, and has no particles in it. She will call her birth attendant and inform him/her that her membranes have released, that she has checked the condition of the fluid, and she will call again when she is closer to moving to the birthing facility. If she discovers her birth show, along with any of the other signs, she will suspect that labor is imminent
She uses Slow Breathing techniques to breathe with her surging body, and she depends upon her baby and her body to let her know that it is time to move to a birthing facility if she is having a hospital or birth center birth.
If she is birthing at home, she will call her midwife and keep her posted as to her progress. She will relax in the comfortable atmosphere of her own home, with its familiar surroundings, and enjoy the ambiance of the place where her baby was conceived.
When the couple arrives at the hospital or other birthing facility, mom will be put onto the EFM for only the 20- minute mandatory reading to establish the baseline for the baby’s heart rate. She will request that her Birth Preference Sheets be reviewed, and that staff refrain from all procedures that could unnecessarily interfere with a normal, undisturbed birth.
She will politely refer to her Birth Preferences as she declines the use of continuous fetal monitoring, preferring intermittent monitoring. She also will decline the IV. The Birth Companion assures the staff that he/she will see to it that mom remains hydrated so there is no need for the insertion of the IV post. Her birth companion will see to it that she remains hydrated and that she snacks. She will request that she be free of the blood pressure cuff between readings if it is inadvertently left behind.
Her birth companion assumes the responsibility for seeing that their Birth Preferences are accommodated in the absence of special circumstances and will remind her to empty her bladder, change positions, and keep hydrated.
Because she is not tethered with belts and monitors, she will be able to move around and to adopt any position she wishes. She may eat and may spend time in the tub for added relaxation. If the couple has rented a birthing tub, and their care provider is on board with their wishes, she may even remain in the tub for birthing, as the benefits of the water in softening the perineum will help the baby’s emergence to go smoothly and gently.
She will be patient and ask for the patience of others. If her membranes have released, she will remain confident and not be frightened into allowing herself to be rushed into augmentation with a synthetic oxytocin. She knows that her baby is not in imminent danger of infection if she has no vaginal exams. She also knows that her vagina does not function like a straw or a sponge. If at least 24 hours pass, she will request antibiotics to ward off the incidence of infection.
If her membranes have not released she will politely decline to allow them to be ruptured because she knows that rupturing the membranes will bring on a more severe labor that will be harder on the baby and will change the nature of her own labor.
If her labor should rest, she will again ask for patience and calm until the labor restarts. She will not be pressured by comments of “failure to progress” if her baby’s heart rate is strong and she is doing well.
She is truly relaxed and trusts her body. Her labor will restart after a rest, and her cervix will open smoothly and easily. She has conditioned herself to go deeper into relaxation and to communicate more with her baby as labor advances. At the end of the opening phase, she will move past completion and go into birthing.
Should her baby be malpositioned (i.e. occiput posterior) she will usually use the Polar Bear position to help reposition the baby, or she will assume the hands and knees position or perhaps use a rebozo. She will spend time talking to her baby to bring about a change. She will maintain her desire for vaginal birth and request that they be given the opportunity to use natural techniques that can help achieve it—patience and relaxation.
Once she has mentally moved into her birthing body, she will follow the lead of her body and her baby and use the Natural Expulsive Reflex (NER) to bring her baby down to crowning. Her baby will be breathed down. She knows that Birth Breathing assists the normal expulsive pulsations of the mom’s body and that a recent study shows that it to be as effective as valsalva pushing. If she experiences an urge to force push, she is able to quiet it with gentle breathing and resume Birth Breathing tomaintain the flow of oxygen to her baby. She knows that vaginal labor is an important part of helping the baby prepare to breathe on the outside.
Her baby will be fully born with no attempt to bulb suction the baby’s nose and mouth, a practice that has been shown in a recent study to be of no benefit in preventing meconium aspiration and not needed under normal circumstances.
Her confidence, and the encouragement of the birth attendant, will help her baby to emerge gently as the tissues of the perineum unfold intact. If the baby’s cord is wrapped around the neck as the baby’s head emerges, a very common occurrence, her birth attendant will gentle remove it.
If it is their preference and arrangements have been made with the birth attendant, the mother will receive her own baby or the birth companion will assist in receiving the baby.
Immediately following the birth, the baby will be placed upon mom’s abdomen, complete with vernix, and the attendant will wait for the cord to stop pulsing before clamping and cutting it.
As part of the bonding that is taking place, she will put her baby to her breast for his first feeding, and mom, dad, and baby will continue to become acquainted. Administrative chores are delayed while the family bonds.
She will experience “rooming in” and have her baby with her throughout her hospital or birth center stay. In some facilities, her birth companion will also remain with the mom, even overnight. If she is at home, her entire family will be a part of the wonderful birth as they all truly experience the celebration of life.
The outcome will be a healthy baby and healthy mother, but also a happy, fulfilled family who have experienced birth, undisturbed and gently. Birthing is about a happy family.
written by the HypnoBirthing institute.



One thought on “Birthing Styles and Approaches”
Perfect post! I am a newly minted natural childbirth instructor and have a difficult time putting mey thoughts into words. This is a fantastic look at a ‘typical’ birth. I will refer my students to this post!